For patients considering Zithromax (azithromycin), it’s crucial to remain informed about the potential risk of ototoxicity. While this antibiotic is primarily used to treat bacterial infections, awareness of its effects on hearing should guide its use, especially in individuals with pre-existing hearing conditions.
Research indicates that high doses of Zithromax may lead to hearing impairment in some patients. Monitoring is essential, particularly for those on extended courses or with kidney dysfunction, as they may be at a heightened risk. Regular hearing assessments can help detect early signs of ototoxicity and allow healthcare providers to adjust treatment accordingly.
Consult with your healthcare professional before starting Zithromax or if you experience any auditory changes during treatment. Early intervention plays a significant role in managing potential adverse effects, safeguarding your hearing health while effectively treating infections.
- Zithromax and Ototoxicity
- Understanding Zithromax: Mechanism of Action
- Impact on Bacterial Infections
- Pharmacokinetics and Tissue Distribution
- Defining Ototoxicity and Its Mechanisms
- Mechanisms of Ototoxicity
- Clinical Evidence Linking Zithromax and Hearing Loss
- Patient Populations at Increased Risk of Ototoxicity
- Recommendations for Monitoring Hearing in Zithromax Users
- Alternative Antibiotics with Lower Ototoxic Risk
- Cefdinir
- Clindamycin
- Implications for Healthcare Providers and Patient Education
Zithromax and Ototoxicity
Zithromax, or azithromycin, is an antibiotic commonly prescribed for various bacterial infections. While it is generally well-tolerated, there are reports linking Zithromax to ototoxicity, which is damage to the ear that affects hearing and balance. Symptoms may include ringing in the ears (tinnitus), hearing loss, or a sense of dizziness.
Monitoring for signs of ototoxicity is advisable, especially in patients with pre-existing ear conditions or those receiving high doses for extended periods. If you notice any auditory disturbances while taking Zithromax, consult your healthcare provider immediately. They may recommend adjustments to your treatment plan or further evaluations.
Current studies suggest the risk of ototoxicity is relatively low compared to other antibiotics, such as aminoglycosides. However, individual susceptibility varies, making personal history an important factor. Be sure to disclose any previous ear issues or adverse reactions to medications when discussing treatment options with your doctor.
In post-treatment evaluations, if hearing loss is detected, audiometric tests may be performed to assess the extent of damage. Patients may need follow-up appointments to monitor their auditory health during and after Zithromax treatment.
Overall, while Zithromax is an effective tool against infection, being proactive about potential side effects, including ototoxicity, helps in managing health risks associated with its use.
Understanding Zithromax: Mechanism of Action
Zithromax, or azithromycin, operates primarily by inhibiting bacterial protein synthesis. By binding to the 50S ribosomal subunit of the bacterial ribosome, it effectively blocks the translocation process of the ribosome during protein synthesis. This action hinders the ability of bacteria to grow and reproduce, leading to their eventual death.
Impact on Bacterial Infections
This antibiotic exhibits a broad spectrum of activity, targeting both Gram-positive and Gram-negative bacteria. Zithromax is particularly effective against common pathogens such as Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Its ability to penetrate tissues and reach high concentrations in sites of infection further enhances its efficacy.
Pharmacokinetics and Tissue Distribution
Zithromax boasts favorable pharmacokinetics, allowing it to maintain therapeutic levels in the body for extended periods. Absorption occurs rapidly after oral administration, with peak plasma concentrations achieved within hours. The drug distributes effectively into various tissues, including lung, tonsil, and middle ear tissues, making it a go-to choice for respiratory and otic infections.
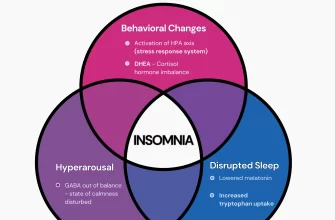
Defining Ototoxicity and Its Mechanisms
Ototoxicity refers to the property of certain medications or chemicals that can damage the inner ear, resulting in hearing loss, tinnitus, or balance issues. This phenomenon may arise from exposure to specific drugs, including some antibiotics, chemotherapy agents, and nonsteroidal anti-inflammatory drugs (NSAIDs). Understanding the mechanisms behind ototoxicity is essential for preventing and managing these adverse effects.
Mechanisms of Ototoxicity
Several mechanisms contribute to ototoxicity. Direct toxicity to hair cells in the cochlea plays a significant role. Aminoglycoside antibiotics, such as gentamicin, cause oxidative stress and disrupt cellular signaling, leading to hair cell death. Increased reactive oxygen species (ROS) may overwhelm the cell’s antioxidant defenses, triggering apoptosis.
Another contributing factor is ototoxic drug accumulation in the inner ear. Certain medications can cross the blood-labyrinth barrier, concentrating within the inner ear fluids, which enhances their toxic effects. Genetic predisposition also influences individual susceptibility to ototoxicity, making some patients more vulnerable to hearing loss when treated with certain drugs.
It’s crucial to monitor patients receiving potentially ototoxic medications. Regular audiological assessments can help detect early signs of hearing damage. Adjusting dosages, switching to less toxic alternatives, or employing protective strategies can mitigate risks associated with ototoxicity.
Clinical Evidence Linking Zithromax and Hearing Loss
Recent studies indicate a potential association between Zithromax (azithromycin) and hearing loss. Clinical observations highlight cases where patients developed hearing impairment following treatment with this antibiotic. A retrospective cohort study published in the “American Journal of Otolaryngology” analyzed data from individuals treated with azithromycin and found a significant increase in reports of hearing loss compared to those who did not receive the medication.
Another notable research effort examined a population of children prescribed Zithromax for respiratory infections. The findings suggested that these patients exhibited higher rates of temporary hearing loss, particularly among those with pre-existing ear conditions. This raises concerns about the drug’s impact on auditory health, particularly in vulnerable populations.
Healthcare providers should remain vigilant when prescribing Zithromax, especially to patients with a history of ear problems. Regular auditory assessments may be advisable for individuals undergoing treatment to detect any changes in hearing status promptly. Patients should also be informed of the potential risks, enabling them to report any symptoms of hearing changes during therapy.
Monitoring and further research are essential to establish a clearer understanding of the relationship between Zithromax use and auditory effects, guiding better clinical practices to protect patients’ hearing health.
Patient Populations at Increased Risk of Ototoxicity
Certain patient populations experience a heightened risk of ototoxicity when using Zithromax. Identifying these groups can significantly enhance patient safety and treatment effectiveness.
- Elderly Patients: Older adults often have pre-existing conditions and may take multiple medications, increasing their vulnerability to ototoxic effects.
- Individuals with Renal Impairment: Reduced kidney function diminishes the body’s ability to eliminate Zithromax, raising the risk of drug accumulation and potential auditory damage.
- Patients with Pre-existing Hearing Loss: Those with any degrees of hearing impairment may experience exacerbated effects, warranting close monitoring during treatment.
- Patients on Concurrent Ototoxic Medications: When prescribed alongside other ototoxic drugs, the risk of combined adverse effects significantly increases.
- Individuals with Previous History of Ototoxicity: A history of reactions to ototoxic agents suggests a predisposition to similar outcomes with Zithromax.
- Pediatric Patients: Children, particularly those younger than two years old, may exhibit increased sensitivity and require careful management when receiving this antibiotic.
Monitoring and careful assessment become vital in these populations. Regular auditory evaluations and dosage adjustments can mitigate risks, ensuring safe and effective treatment outcomes.
Recommendations for Monitoring Hearing in Zithromax Users
Regular hearing assessments are vital for individuals taking Zithromax. Schedule audiological evaluations before starting treatment and periodically during and after completion. This proactive approach allows for timely identification of any auditory changes.
Follow up with your healthcare provider if you notice any signs of hearing loss or tinnitus while on Zithromax. Symptoms may include ringing in the ears, muffled hearing, or difficulty understanding conversations. Prompt communication can help address issues early.
Consider routine self-checks for hearing sensitivity. Pay attention to how well you hear soft sounds or conversations in noisy environments. Keeping a log of any auditory changes can provide useful information for your healthcare professional.
Discuss any pre-existing conditions with your doctor. Conditions such as prior ototoxicity, ear infections, or hearing loss may necessitate closer monitoring. Collaborating with your healthcare provider ensures a tailored monitoring plan suited to your specific needs.
Encourage family members or close friends to observe any changes in your hearing. Their insights may help detect subtle shifts that you might overlook. Open communication aids in early detection and intervention.
Explore using assistive listening devices if significant changes occur. These tools can enhance communication effectiveness and maintain quality of life while managing any auditory challenges.
Stay informed about your medications. Some drugs can interact with Zithromax and heighten the risk of hearing issues. Regularly review your medication list with your healthcare provider to ensure safety.
Alternative Antibiotics with Lower Ototoxic Risk
Amoxicillin and its derivatives are strong candidates when considering antibiotics with a lower risk of ototoxicity. This class of antibiotics effectively treats various bacterial infections without the potential auditory side effects associated with Zithromax. Prescribing amoxicillin allows the management of infections such as sinusitis and otitis media without compromising hearing health.
Cefdinir
Cefdinir is another excellent alternative. It belongs to the cephalosporin class and is highly effective against respiratory tract infections. This antibiotic comes with a favorable safety profile, minimizing the risk of ototoxic effects while providing broad-spectrum coverage.
Clindamycin
Clindamycin also offers an effective solution, particularly for skin and soft tissue infections. Its mechanism targets various bacteria while maintaining a low incidence of ototoxicity, allowing for safe use in patients concerned about hearing loss.
| Antibiotic | Indications | Ototoxic Risk |
|---|---|---|
| Amoxicillin | Respiratory tract infections, otitis media | Low |
| Cefdinir | Respiratory tract infections | Low |
| Clindamycin | Skin and soft tissue infections | Low |
Selecting these alternatives can significantly reduce concerns about ototoxicity while effectively tackling bacterial infections. Always consult with a healthcare professional to determine the most appropriate antibiotic for your specific condition.
Implications for Healthcare Providers and Patient Education
Monitor patients receiving Zithromax closely for signs of ototoxicity, particularly if they have pre-existing hearing issues or are taking other ototoxic medications. Regular hearing assessments can aid in early detection of auditory complications.
Educate patients about potential risks associated with Zithromax. Provide clear information on symptoms of ototoxicity, such as tinnitus, hearing loss, or dizziness. Encourage them to report any such symptoms immediately.
- Discuss alternative antibiotics if the risk of ototoxicity is a concern.
- For patients with known ototoxicity risks, collaborate with audiologists to create a monitoring plan.
- Ensure that patients understand the importance of completing the full course of antibiotics unless otherwise directed.
Use visual aids or pamphlets to convey information about Zithromax and its side effects. Tailor educational materials to match the patient’s literacy level and understanding.
Incorporate discussions about ototoxicity into routine follow-ups, reinforcing the importance of monitoring and awareness. Address any concerns patients may have about hearing-related issues promptly.
Provide support for patients experiencing side effects. Offer guidance on coping strategies, including referrals to support groups or counseling services as needed. This holistic approach can enhance their overall healthcare experience.