Monitor patients closely taking prednisone, as they may face an increased risk of pulmonary embolism. Prednisone, a corticosteroid, is commonly used for its anti-inflammatory properties. However, its use can alter various physiological responses, leading to potential complications, including thromboembolic events.
Research indicates that corticosteroids like prednisone can influence factors such as blood coagulation and endothelial function. These changes may predispose individuals to venous thromboembolism, including pulmonary embolism. Close observation of clinical signs, such as shortness of breath, chest pain, and swelling in the legs, is crucial for early detection.
Healthcare providers must assess the risk factors for each patient, including any history of thromboembolic disease, recent surgeries, or prolonged immobility. Consider preventive measures like anticoagulation therapy for those with significant risk factors, especially during prolonged prednisone therapy.
- Prednisone and Pulmonary Embolism
- Risk Factors to Consider
- Symptoms of Pulmonary Embolism
- Understanding the Mechanism of Action of Prednisone in Treating Inflammatory Conditions
- Risk Factors for Pulmonary Embolism in Patients Using Prednisone
- Clinical Considerations and Management Strategies for Patients with Pulmonary Embolism on Prednisone
- Assessment and Diagnosis
- Management Strategies
Prednisone and Pulmonary Embolism
Patients taking prednisone should be aware of its potential impact on thromboembolic events, including pulmonary embolism (PE). Prednisone can increase the risk of blood clots due to its effects on blood viscosity and coagulation. Monitoring is crucial for those on long-term corticosteroid therapy, especially if they have other risk factors such as obesity, recent surgery, or a history of clotting disorders.
Risk Factors to Consider
Evaluate individual risk factors carefully. Prednisone users should consider their personal and family history of venous thromboembolism. Patients with additional conditions such as heart disease, cancer, or prolonged immobility face a higher risk. Engaging in regular physical activity, maintaining adequate hydration, and avoiding smoking can help mitigate these risks. Consult healthcare providers for tailored advice on balancing prednisone treatment and PE risks.
Symptoms of Pulmonary Embolism
Be vigilant for symptoms indicative of pulmonary embolism, including sudden shortness of breath, chest pain, or rapid heartbeat. These signs warrant immediate medical attention. Early diagnosis of PE significantly enhances treatment outcomes. Individuals on prednisone should proactively communicate any concerning symptoms to their healthcare provider to ensure swift evaluation and intervention.
Understanding the Mechanism of Action of Prednisone in Treating Inflammatory Conditions
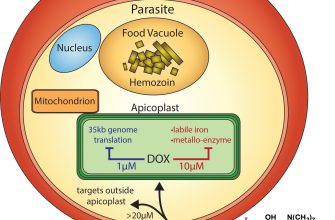
Prednisone effectively reduces inflammation by mimicking the action of natural hormones produced by the adrenal glands. This corticosteroid inhibits the release of substances in the body that cause inflammation, leading to decreased swelling and tissue damage.
Upon administration, prednisone gets converted into its active form, prednisolone, in the liver. This conversion allows it to bind to glucocorticoid receptors in the cytoplasm of cells. Once bound, the receptor complex translocates to the nucleus, where it initiates a series of genetic mechanisms that suppress the expression of pro-inflammatory proteins and promote the expression of anti-inflammatory proteins.
Prednisone also influences immune responses. It reduces the proliferation and activity of lymphocytes, which are crucial in mediating the immune response. By decreasing the number of white blood cells and suppressing their function, prednisone ameliorates various autoimmune and inflammatory diseases.
Additionally, this medication stabilizes cell membranes, which limits the release of enzymes that further propagate inflammation. It inhibits the phospholipase A2 enzyme, decreasing the synthesis of inflammatory mediators like prostaglandins and leukotrienes.
In treating conditions such as asthma, rheumatoid arthritis, and inflammatory bowel disease, prednisone can provide rapid symptom relief, allowing for improved quality of life. However, use should be closely monitored due to potential side effects, including immunosuppression and metabolic changes.
Understanding these mechanisms helps guide effective treatment strategies while minimizing risks associated with long-term use. Always consult with healthcare professionals for personalized advice regarding prednisone therapy.
Risk Factors for Pulmonary Embolism in Patients Using Prednisone
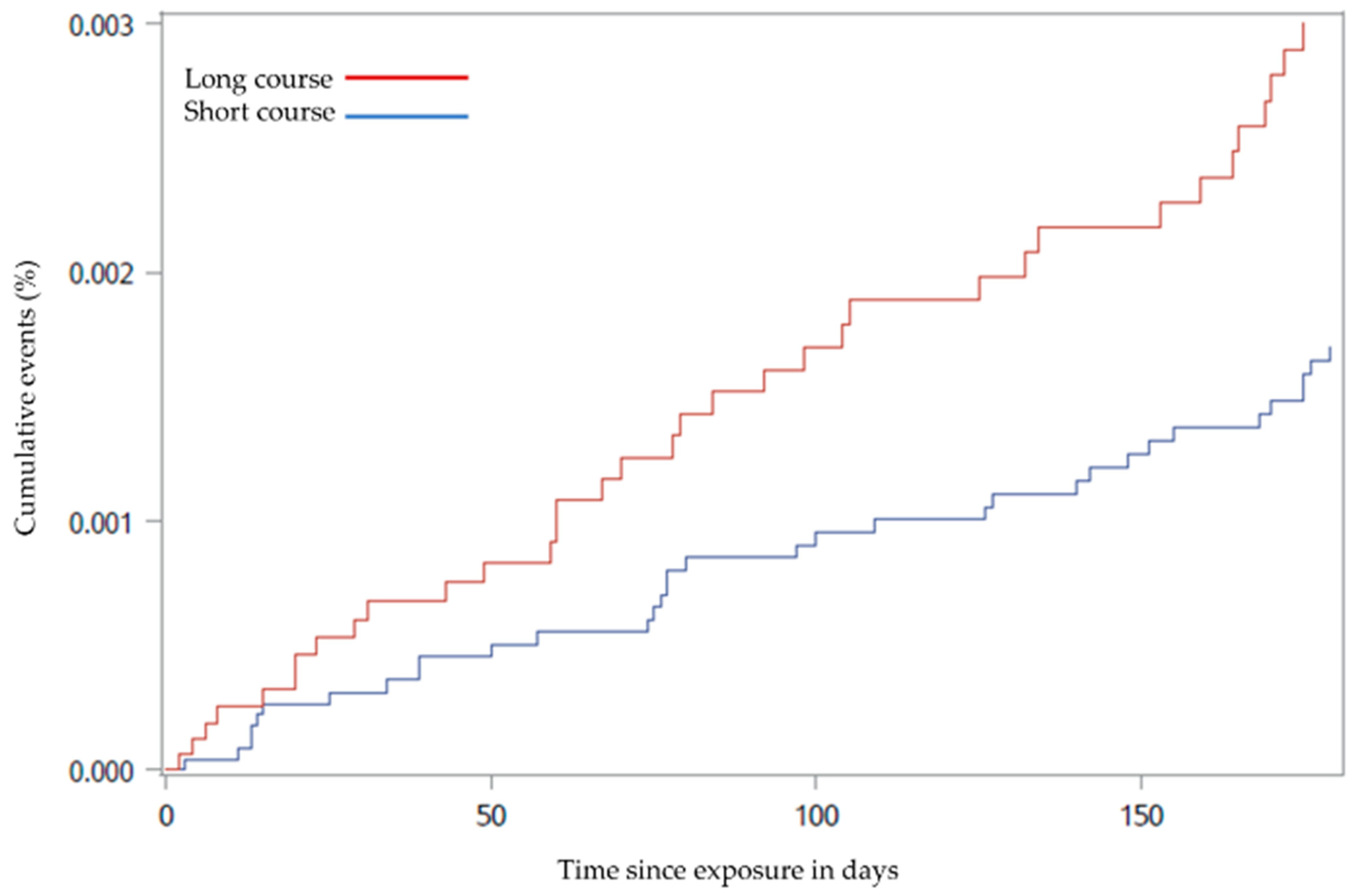
Patients using prednisone should be aware of several key risk factors for pulmonary embolism (PE). Notably, prolonged steroid use can lead to various complications that heighten the likelihood of PE. These factors include obesity, prolonged immobility, history of venous thromboembolism, and other co-existing medical conditions.
Obesity significantly increases the risk of thrombosis. The accumulation of fat can lead to pressure on veins, slowing blood flow and promoting clot formation. Maintaining a healthy weight is advisable. Regular exercise mitigates the risks related to immobility. Encourage activities that enhance circulation, especially during long periods of inactivity.
Patients with a history of venous thromboembolism are at greater risk. Monitor for signs of clots, and seek medical advice about preventive measures. Additionally, those with conditions such as cancer, heart disease, or respiratory issues should manage their health proactively, as these can contribute to a higher risk of PE.
It is essential to consider factors such as age and hormonal influences. Older adults and women using estrogen-containing medications can face increased susceptibility. Regular check-ups can facilitate monitoring and early intervention if necessary.
| Risk Factor | Description |
|---|---|
| Obesity | Excess weight impacts vein pressure, slowing blood flow. |
| Prolonged Immobility | Reduced movement increases thrombosis risk. |
| History of Thrombosis | Prior clots elevate future risk; monitor closely. |
| Co-existing Medical Conditions | Conditions like cancer or heart disease heighten risk. |
| Age | Older adults have a natural increase in risk factors. |
| Hormonal Factors | Estrogen therapies can impact clotting risks. |
Regular communication with healthcare providers helps tailor individual risk management strategies. Awareness of these risk factors enables proactive measures, contributing to safer outcomes for those using prednisone.
Clinical Considerations and Management Strategies for Patients with Pulmonary Embolism on Prednisone
Monitor for increased risk of thromboembolism due to potential hypercoagulable state from prednisone use. Assess the patient’s current therapy, specifically the dosage and duration of corticosteroid treatment, and its correlation with susceptibility to thrombotic events.
Assessment and Diagnosis
- Perform imaging studies such as CT pulmonary angiography to confirm pulmonary embolism.
- Evaluate D-dimer levels, though they can be elevated with corticosteroid therapy.
- Review patient history for additional risk factors, including obesity, previous thromboembolic events, and other medications that may contribute to coagulation changes.
Management Strategies
- Consider anticoagulation therapy for patients diagnosed with pulmonary embolism. Select agents based on individual risk factors and contraindications.
- If the patient is already on prednisone for an underlying condition, discuss with the healthcare team the possibility of adjusting corticosteroid dosages.
- Educate patients on signs and symptoms of potential complications, including worsening respiratory distress or symptoms of recurrent thrombosis.
Collaborate with specialists, such as pulmonologists, and consider multidisciplinary approaches for comprehensive care. Regular follow-ups are necessary to assess the patient’s response to treatment and adjust management plans accordingly.