Yes, prednisone is classified as an immunosuppressant drug. It functions by inhibiting the immune system’s response, making it effective in treating various autoimmune conditions and inflammatory diseases. By dampening the activity of the immune system, prednisone reduces inflammation and helps manage symptoms in conditions such as rheumatoid arthritis, lupus, and certain allergic reactions.
Understanding how prednisone affects your body is vital, especially if you’re considering its use for chronic health issues. It alters the function of immune cells, specifically lymphocytes, diminishing their ability to respond to perceived threats. This can lead to reduced inflammation but also increases susceptibility to infections.
In some cases, healthcare professionals prescribe prednisone to manage organ transplant recipients’ immune responses, ensuring that the body does not reject the new organ. While it can be a powerful tool in managing certain health conditions, monitoring for potential side effects is crucial. Always consult with your healthcare provider before beginning or discontinuing this medication to ensure safe and effective use.
- Is Prednisone an Immunosuppressant Drug?
- Understanding Prednisone and Its Uses in Medicine
- Indications for Use
- Administering Prednisone Safely
- Mechanism of Action: How Prednisone Functions as an Immunosuppressant
- Effects on Immune Cells
- Impact on Inflammatory Pathways
- Risks and Side Effects of Using Prednisone as an Immunosuppressant
- Common Side Effects
- Serious Risks
- Alternatives to Prednisone in Immunosuppressive Therapy
- Azathioprine
- Biologics
Is Prednisone an Immunosuppressant Drug?
Yes, prednisone acts as an immunosuppressant drug. It reduces the immune system’s response, which can benefit individuals with autoimmune diseases, allergies, and certain inflammatory conditions.
Prednisone mimics the effects of cortisol, a hormone produced by the adrenal glands. By suppressing the activity of white blood cells and decreasing inflammation, it effectively manages symptoms associated with various disorders.
This medication is frequently used in conditions like rheumatoid arthritis, lupus, and asthma, where dampening the immune response can alleviate symptoms and improve quality of life. It is important to follow prescribed dosages and consult healthcare providers, as long-term use can lead to side effects such as increased risk of infections and weight gain.
Gradual tapering of the drug is often necessary to avoid withdrawal symptoms, as the body may struggle to resume natural cortisol production. Regular monitoring by healthcare professionals ensures the safe use of prednisone while maximizing treatment benefits.
Understanding how prednisone interacts with the immune system is crucial for patients and caregivers. By recognizing its immunosuppressive properties, individuals can make informed decisions regarding their treatment plans and lifestyle adjustments. Always discuss potential risks and benefits with a healthcare provider before making any changes to medication regimens.
Understanding Prednisone and Its Uses in Medicine
Prednisone is a powerful synthetic corticosteroid commonly prescribed to reduce inflammation and suppress the immune system. This medication is effective in treating various conditions such as autoimmune diseases, allergies, and asthma. Physicians often recommend prednisone for its ability to quickly control symptoms and improve the quality of life for patients suffering from chronic illnesses.
Indications for Use
Healthcare providers frequently use prednisone for conditions like rheumatoid arthritis, lupus, and multiple sclerosis. It helps manage flares and maintain remission by alleviating inflammation. In cases of severe allergic reactions or asthma exacerbations, prednisone acts swiftly to reduce airway inflammation and improve breathing. Its role in transplant medicine is significant, as it prevents organ rejection by suppressing the body’s immune response.
Administering Prednisone Safely
Starting doses of prednisone vary based on the specific condition and severity. It is crucial to follow a doctor’s directions carefully. Gradual tapering off the drug is often necessary to minimize potential withdrawal symptoms and allow the body’s natural cortisol production to resume. Regular medical check-ups are advisable to monitor side effects, including weight gain, mood changes, and increased blood sugar levels, especially in long-term use.
Mechanism of Action: How Prednisone Functions as an Immunosuppressant
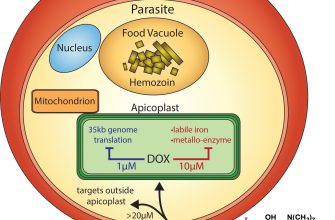
Prednisone works as an immunosuppressant by mimicking the actions of cortisol, a hormone produced by the adrenal glands. It binds to glucocorticoid receptors in various cells, altering gene expression and modulating the immune response. This interaction leads to a decrease in the production of pro-inflammatory cytokines, effectively reducing inflammation and immune activity.
Effects on Immune Cells
When prednisone enters the bloodstream, it circulates and easily penetrates cell membranes. Once inside, it influences several immune cells, including lymphocytes and macrophages. By downregulating the activation of T-cells and inhibiting the proliferation of B-cells, prednisone limits the overall immune response. This results in reduced antibody production and less immune activity against perceived threats.
Impact on Inflammatory Pathways
Prednisone also interrupts key inflammatory pathways. It inhibits the release of arachidonic acid from cell membranes, which leads to decreased synthesis of prostaglandins and leukotrienes, both of which play significant roles in inflammation. Additionally, it suppresses the expression of cyclooxygenase enzymes, further limiting inflammatory responses. These combined actions contribute to the medication’s therapeutic effects in managing autoimmune diseases and preventing organ transplant rejection.
Risks and Side Effects of Using Prednisone as an Immunosuppressant
Prednisone can lead to several risks and side effects when used as an immunosuppressant. Understanding these effects helps in managing treatment effectively.
Common Side Effects
- Weight gain due to increased appetite.
- Fluid retention, causing swelling in legs and abdomen.
- Elevated blood sugar levels, potentially triggering diabetes.
- Insomnia and changes in mood, including anxiety or depression.
- Prolonged use may result in osteoporosis, increasing fracture risk.
Serious Risks
- Increased susceptibility to infections due to lowered immune response.
- Gastrointestinal issues, such as ulcers or gastrointestinal bleeding.
- Cardiovascular complications, including hypertension and heart disease.
- Adrenal insufficiency, which can occur if the medication is abruptly discontinued.
- Cushing’s syndrome, characterized by weight gain, rounded face, and skin changes.
Regular monitoring by a healthcare provider is essential. Discuss any unexpected symptoms or significant side effects immediately. Adjustments may be necessary to balance the benefits of treatment against these risks.
Alternatives to Prednisone in Immunosuppressive Therapy
Consider methotrexate as a strong alternative to prednisone for immunosuppressive therapy. It effectively reduces inflammation and suppresses the immune response, making it suitable for patients with rheumatoid arthritis and certain autoimmune disorders. Methotrexate is often preferred due to its lower side effect profile compared to long-term prednisone use.
Azathioprine
Azathioprine stands out for its ability to suppress immune responses without the significant adrenal suppression associated with prednisone. Frequently used in organ transplantation and autoimmune diseases like lupus, azathioprine can offer a more stable long-term solution for managing immune activity. Monitoring liver enzymes and blood counts is essential during treatment to mitigate potential side effects.
Biologics
Biologic therapies, such as abatacept and rituximab, provide targeted immune modulation. These agents focus on specific components of the immune system, offering effective treatment for conditions like rheumatoid arthritis and psoriasis. They can reduce the need for corticosteroids like prednisone and lessen the risk of systemic side effects. Patients should discuss with their healthcare providers to determine the best machine for their condition.