Carefully monitor patients using chloramphenicol for signs of toxicity, as this antibiotic can lead to serious side effects, particularly aplastic anemia. Regular blood tests are essential to track white blood cell counts and detect any abnormalities early.
Chloramphenicol’s mechanism of action interferes with protein synthesis in bacteria, but it can also impact bone marrow function. Patients should be informed about symptoms like fever, sore throat, and unusual bruising or bleeding, which may indicate hematologic complications.
Be mindful of drug interactions, especially with medications that may further suppress bone marrow. Adjustments to dosages or alternative therapies may be necessary to minimize risks. Establish a clear communication line between healthcare providers and patients to ensure swift reporting of any adverse effects.
- Chloramphenicol Toxicity
- Symptoms and Risk Factors
- Management Strategies
- Understanding Chloramphenicol: An Overview
- Mechanism of Action and Pharmacokinetics
- Pharmacokinetics
- Half-Life and Excretion
- Clinical Uses of Chloramphenicol
- Identifying Symptoms of Chloramphenicol Toxicity
- Common Symptoms
- Severe Reactions
- Risk Factors for Chloramphenicol Toxicity
- Laboratory Tests to Diagnose Chloramphenicol Toxicity
- Blood Levels of Chloramphenicol
- Liver Function Tests
- Management and Treatment of Chloramphenicol Toxicity
- Preventive Measures and Guidelines for Safe Use
- Monitoring and Dosage
- Avoiding Drug Interactions
Chloramphenicol Toxicity
Monitor patients closely for signs of bone marrow suppression and allergic reactions when administering chloramphenicol. Regular complete blood counts (CBC) help detect these issues early. Patients may experience aplastic anemia, which can be life-threatening. Be vigilant about any unusual bruising, bleeding, or fatigue, and take necessary action if these signs arise.
Symptoms and Risk Factors
Symptoms of chloramphenicol toxicity include nausea, vomiting, and diarrhea. More serious effects involve cardiovascular issues and severe allergic reactions such as anaphylaxis. Patients with pre-existing bone marrow disorders or those receiving other medications that affect liver function are at a heightened risk. Therefore, always evaluate a patient’s complete medical history before treatment.
Management Strategies
Discontinue chloramphenicol immediately if any signs of toxicity occur. Supportive care, including fluids and monitoring vital signs, can improve outcomes. Consider hematology consultation for patients demonstrating significant hematologic abnormalities. Educate patients to report any symptoms promptly, ensuring timely intervention. Always weigh the benefits against the risks when deciding on chloramphenicol use.
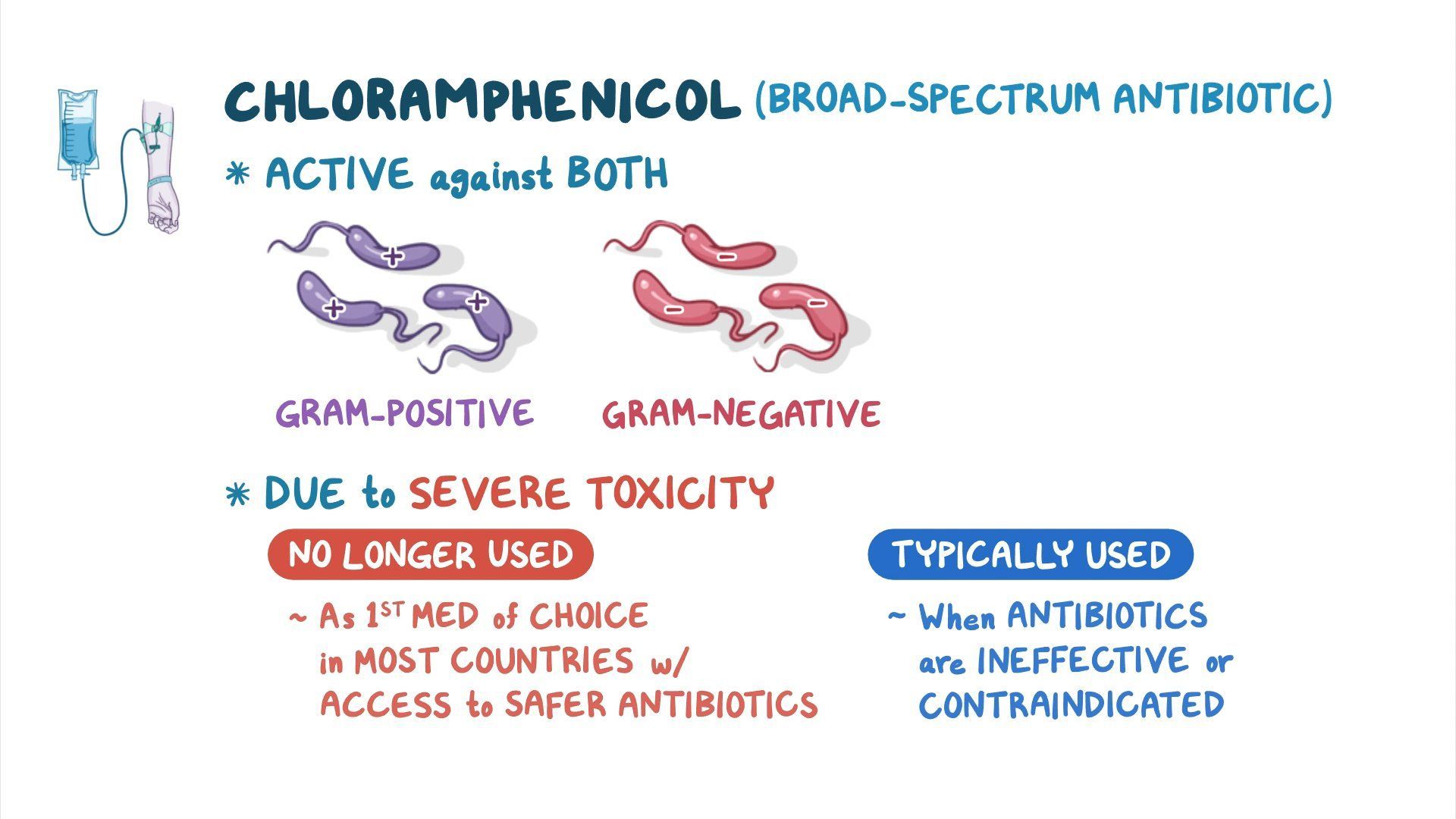
Understanding Chloramphenicol: An Overview
Chloramphenicol serves as a powerful antibiotic primarily effective against gram-negative and gram-positive bacteria. Originally isolated from Streptomyces venezuelae, it is synthetically produced today for clinical use.
This antibiotic disrupts bacterial protein synthesis by binding to the 50S ribosomal subunit, interfering with peptide bond formation. Its broad-spectrum capabilities treat a variety of infections, including typhoid fever and bacterial meningitis, showcasing its clinical value.
However, chloramphenicol poses significant toxicity risks. Rare but serious conditions like aplastic anemia, gray baby syndrome, and dose-related bone marrow suppression require cautious administration. Routine monitoring of blood parameters is advised when utilizing this medication to ensure patient safety.
Understanding potential interactions with other drugs enhances treatment outcomes. Chloramphenicol can intensify the effects of anticoagulants and may reduce the efficacy of certain vaccines, making careful medication management essential.
Clinicians should reserve chloramphenicol for situations where alternative antibiotics are ineffective or contraindicated. Always evaluate the risk-to-benefit ratio based on individual patient circumstances. Engage patients in discussions regarding side effects and encourage them to report any unusual symptoms promptly.
In summary, chloramphenicol remains a valuable antibiotic when handled judiciously. Its application demands careful consideration of benefits versus potential adverse effects, advocating for informed clinical decisions and patient education.
Mechanism of Action and Pharmacokinetics
Chloramphenicol inhibits bacterial protein synthesis by binding to the 50S subunit of the ribosome. This action prevents the formation of peptide bonds and disrupts the elongation of the polypeptide chain during translation. As a result, bacterial growth is effectively halted. This mechanism primarily affects Gram-positive and Gram-negative bacteria, making chloramphenicol a broad-spectrum antibiotic.
Pharmacokinetics
Chloramphenicol absorbs rapidly and completely after oral administration. Its bioavailability exceeds 90%, allowing for effective serum concentrations with standard doses. The drug distributes widely throughout the body, penetrating tissues, including the central nervous system, which is crucial for treating certain infections like meningitis. Chloramphenicol undergoes metabolism primarily in the liver through glucuronidation, leading to both active and inactive metabolites. This metabolic pathway can vary significantly among individuals, influencing dosing strategies.
Half-Life and Excretion
The half-life of chloramphenicol averages around 1 to 3 hours in healthy individuals, but it can extend significantly in those with liver dysfunction. Renal excretion plays a minor role in its elimination; however, patients with compromised liver function may require dosage adjustments. Monitoring serum levels helps mitigate the risk of toxicity, particularly in prolonged therapy.
Clinical Uses of Chloramphenicol
Chloramphenicol is primarily utilized for its broad-spectrum antibacterial properties, particularly against severe bacterial infections where other antibiotics may not be effective. It is often reserved for critical cases due to its potential toxicity.
The drug is indicated for treating typhoid fever, caused by Salmonella typhi, especially in patients who cannot tolerate or have resistant strains. Also, it remains a viable option for certain cases of meningitis, particularly caused by Haemophilus influenzae and Neisseria meningitidis.
Chloramphenicol is particularly useful in treating severe eye infections like bacterial conjunctivitis and keratitis, delivered via topical formulations. Its penetration into ocular tissues is advantageous in such instances.
In addition to bacterial infections, chloramphenicol sometimes treats rickettsial infections, including typhus. It serves as a reliable alternative in patients with penicillin allergies when treating infections caused by susceptible organisms.
Moreover, chloramphenicol plays a role in the treatment of some zoonotic infections, where other antibiotics may not have the same efficacy. It may also be used empirically when the causative organism is unknown, particularly in cases of severe sepsis.
Below is a summary of the clinical applications of chloramphenicol:
| Indication | Pathogen | Formulation |
|---|---|---|
| Typhoid Fever | Salmonella typhi | Oral/IV |
| Meningitis | Haemophilus influenzae, Neisseria meningitidis | IV |
| Bacterial Conjunctivitis | Various bacteria | Topical |
| Rickettsial Infections | Rickettsia spp. | Oral/IV |
| Zoonotic Infections | Various pathogens | Oral/IV |
Due to the possibility of serious side effects, careful consideration and monitoring are essential when using chloramphenicol in clinical practice. Its application remains crucial in specific scenarios where alternative treatments are inadequate or contraindicated.
Identifying Symptoms of Chloramphenicol Toxicity
Watch for specific symptoms when assessing chloramphenicol toxicity. Early detection can lead to effective management and treatment options.
Common Symptoms
- Aplastic Anemia: Signs include fatigue, weakness, and increased susceptibility to infections.
- Bone Marrow Suppression: Monitor for bruising, prolonged bleeding, and unusual paleness.
- Gastrointestinal Distress: Nausea, vomiting, and diarrhea may occur.
- Liver Dysfunction: Jaundice, dark urine, and abdominal pain are key indicators.
Severe Reactions
- Gray Baby Syndrome: Watch for lethargy, poor feeding, and a grayish tint to the skin in newborns treated with chloramphenicol.
- Allergic Reactions: Look for rash, itching, or swelling, especially after recent exposure.
Regular monitoring and prompt medical attention can significantly mitigate risks associated with chloramphenicol toxicity. If any of these symptoms arise, seek help immediately.
Risk Factors for Chloramphenicol Toxicity
Patients with specific conditions should be closely monitored when prescribed chloramphenicol. Age can significantly influence toxicity; neonates and infants demonstrate higher susceptibility due to their underdeveloped liver enzymes. Ensure that healthcare providers evaluate the patient’s age before administration.
Prior history of bone marrow suppression also increases the risk. Patients with existing hematological conditions, such as aplastic anemia, should avoid chloramphenicol unless absolutely necessary. Regular blood work can aid in detecting any changes in blood count during treatment.
Underlying liver or kidney dysfunction exacerbates the risk of toxicity. A thorough assessment of renal and hepatic function is advisable prior to initiating therapy. Adjusting dosages or exploring alternative treatments may be warranted based on test results.
Concurrent use of other medications also heightens the potential for adverse effects. Some drugs may interact with chloramphenicol, amplifying its toxicity. Always review the full medication list, including over-the-counter and herbal supplements, to avert any harmful combinations.
Genetic factors can play a role; individuals with specific genetic polymorphisms may experience increased susceptibility to adverse reactions. Genetic screening may be beneficial in high-risk populations.
Patients receiving prolonged courses of chloramphenicol should be evaluated regularly for signs of toxicity. An ongoing assessment of clinical symptoms and laboratory markers ensures timely intervention and management of potential complications.
| Risk Factor | Recommendation |
|---|---|
| Age (Neonates & Infants) | Monitor closely; consider alternative treatments. |
| Bone Marrow Suppression History | Avoid use if possible; conduct regular blood tests. |
| Liver or Kidney Dysfunction | Assess function prior to treatment; adjust dosages. |
| Concurrent Medications | Review all medications to prevent interactions. |
| Genetic Factors | Consider genetic screening for high-risk individuals. |
| Prolonged Therapy | Regular clinical evaluation and lab monitoring. |
Laboratory Tests to Diagnose Chloramphenicol Toxicity
Conduct a complete blood count (CBC) to evaluate for bone marrow suppression, a common consequence of chloramphenicol toxicity. Look for leukopenia, thrombocytopenia, and anemia. These parameters indicate the impact of chloramphenicol on hematopoiesis.
Blood Levels of Chloramphenicol
Measure plasma levels of chloramphenicol through high-performance liquid chromatography (HPLC). Identify elevated concentrations that can signify toxicity, especially in patients presenting with symptoms.
Liver Function Tests
Perform liver function tests (LFTs) to assess potential hepatotoxicity. Monitor alanine aminotransferase (ALT), aspartate aminotransferase (AST), and bilirubin levels for any deviations that might indicate hepatic involvement in the toxicity.
Management and Treatment of Chloramphenicol Toxicity
Administer activated charcoal if ingestion occurred within one hour. This step reduces systemic absorption of chloramphenicol. Monitor the patient’s vital signs closely, noting any signs of respiratory distress or altered consciousness. Ensure intravenous access for fluid and electrolyte management.
Perform complete blood counts regularly to assess for bone marrow suppression, a significant risk associated with chloramphenicol toxicity. Leukopenia or aplastic anemia may require transfusions or supportive therapy.
For patients experiencing significant hypotension, initiate fluid resuscitation. Consider the use of vasopressors if fluid therapy fails to stabilize blood pressure. Continuously evaluate the patient’s cardiovascular status.
- Administer antibiotics if infection occurs secondary to neutropenia.
- Monitor liver function tests on a weekly basis to detect potential hepatotoxicity.
- Evaluate renal function periodically, as chloramphenicol can cause nephrotoxicity.
In severe cases of toxicity, consider the use of hematopoietic growth factors to stimulate blood cell production. Coordinate care with a toxicologist or a medical toxicology specialist for advanced management strategies.
Patient education is essential. Explain the signs of potential toxicity and the importance of reporting any unusual symptoms, such as fever or bleeding. Encourage adherence to follow-up appointments to monitor blood counts and overall health.
Preventive Measures and Guidelines for Safe Use
Always obtain chloramphenicol through a licensed medical professional. This ensures the medication is appropriate for the specific infection and patient condition. Avoid self-medication or using leftover prescriptions.
Monitoring and Dosage
Monitor for side effects, particularly during the first few days of treatment. Adjust dosages based on kidney function and other health parameters. Regularly check blood counts to identify early signs of bone marrow suppression.
Follow prescribed doses strictly and never exceed them. Dividing doses throughout the day can help maintain effective drug levels without overwhelming the system.
Avoiding Drug Interactions
Review all medications with a healthcare provider to identify potential interactions. Steer clear of using chloramphenicol with drugs known to affect bone marrow or liver function. Always disclose any other treatments or supplements being taken.
Educate patients about the signs of adverse reactions, such as fever, sore throat, or unusual bruising, and advise them to seek immediate medical attention if these occur.